Bizzell Responds to the Opioid Crisis
A Message About the Opioid Crisis
From Anton C. Bizzell, M.D.
Bizzell, President & Chief Executive Officer
Transcript
[Anton C. Bizzell] The opioid crisis in
the United States, driven largely by illicitly obtained synthetic
opioids such as fentanyl, is impacting communities and
families across the country and is far from being over.
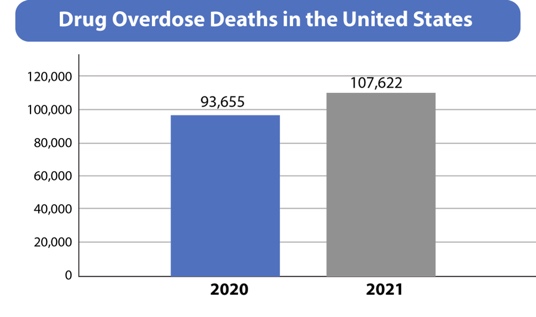
From December 1999 to June 2023,
opioid related overdose deaths increased 100 and threefold.
Hardly a day goes by when there
isn’t a news item about a family losing a loved one on illicit
fentanyl seizure. A recent fentanyl seizure by
California police of 4.2 kilos was enough to potentially kill
2.1 million people. Significant spikes in the US
overdose crisis are linked to poly substance use of synthetic
compounds such as xylazine, a veterinary tranquilizer.
Xylazine extends the duration of
action of fentanyl but does not respond to naloxone.
If an overdose occurs, it is
also associated with an increased risk of soft tissue
infections. Fentanyl impacts minorities at
an alarming rate, with overdose rates among non Hispanic blacks
suffering the highest mortality due to synthetic opioids other
than methadone. A new CDC report shows that more
black Americans died from fentanyl overdoses than any
other drug in 2021 and at a far higher rate than whites or
Hispanics. As a minority owned business,
Bizzell is committed to providing solutions to address
the current opioid crisis. At Bizzell US, all employees are
required to watch a brief training on a five step response
to an opioid overdose and are encouraged to carry naloxone
with them to stress the wide-ranging impact of the
opioid epidemic or frontline providers. Bizzell has created a
testimonial video with descriptions of the difficulties
and heart breaks of managing the opioid crisis as well as the
importance of treatment initiation in emergency
departments. An additional story about
fentanyl test strips comes from an emergency department
physician. As his daughter was heading off
to college. He taught her how to use
fentanyl test strips just in case. His foresight saved many lives
at a campus party because of this knowledge.
Bizzell US is proud to have created a variety of tools and
resources for public use in conjunction with the National
Institute on Drug Abuse Clinical Trials Network Dissemination
Initiative, bringing research based information to clinicians
on a variety of topics related to substance use disorders.
I invite you to take the time to
review all of these important resources. There is hope. With dedicated
professionals across the United States and around the world,
Bizzell is working to help turn around the opioid crisis which
effects all of us. Please join us in our efforts by
getting trained in how to recognize and manage an opioid
overdose and carry naloxone with you so you can be a first
responder. Also, please encourage anyone
you know who is using opioids to seek treatment.
Thank you.
Responding to an Overdose
This 5–step response to a possible opioid overdose, which encourages using 911 for immediate assistance and recommends that everyone carry naloxone is a quick and accessible resource.
Transcript
[Maia Brown] If you come across someone with
an opiate overdose, I’d like to share with you how you can help
in five easy steps.
Step one. Check for signs of
opiate overdose. Remember that these patients
have pinpoint pupils and decreased respiratory drive,
meaning they’re breathing less than 5 times a minute or not at all. You may also see signs of drug
use on scene, like pills on the ground or an IV needle sticking
out of their arm.
Step two. Call 911 so we can
come and help you.
Step three. If you have
naloxone, go ahead and give it. You will not hurt the patient by
trying to give this medication.
Step four. Help the patient with
their breathing. If they’re not already on their
back, roll them onto their back and put them in a sniffing
position so that they have a nice open airway. Remember that naloxone can cause
patients to vomit, in which case roll them onto their side into
the recovery position.
Step 5. Continue to monitor the patient
and look for any changes in how they present to you and wait for
help to arrive. That’s all there is to it. Thank you for being willing to
help.
Personal Testimonials
Testimonials from front line community providers stress the wide-ranging impact of the opioid crisis. Each clip describes the difficulties and heartbreaks of managing the crisis while offering hope and stressing the importance of treatment initiation in Emergency Departments.
Transcript
[Ben Savitch] I worked for many years in inner
city hospitals in Chicago, and I remember distinctly one shift
many years ago where I was working in the overnight shift
and in the morning I looked up from my computer station and I
saw that our emergency department was overwhelmed with
people that were there due to opioid overdoses. Many of these individuals had
received Narcan in the field by EMS and additional doses in the
emergency department. And that was really a
recognition point for me that we were immersed in this epidemic. And certainly the issue has
persisted and extends across our entire country.
[Angadpreet “Preet” Sidhu] My community
has been disproportionately affected by the opiate crisis. Earlier this year, New York City
Health and Hygiene released their 2021 data on overdose
deaths. One particular statistic was
breakdown by neighborhood. Metropolitan Serves East Harlem,
which ranked #5 in neighborhoods with overdose deaths in all of
New York City for 100,000 residents #6 on the list was
Harlem neighborhood served by my hospital, Harlem Hospital.
[Alan Grow] They asked that any members of
the community that know of anybody struggling with
addiction to any sort of drug or alcohol, please get them help. The most important thing is
getting these people help, realizing that the stuff that
they’re doing is not only bad for them, but it’s going to harm
somebody else.
[Kavita Babu] I think it’s a real testament
to emergency medicine how much our care of patients with a opioid
use disorder has changed in my more than 20 years in practice. When I started, we would simply
give patients a handout advising them not to use drugs, but now
we’re able to send them out of our emergency departments with
things like buprenorphine, naloxone or Suboxone, meloxone
or Narcan, as well as harm reduction supplies and won’t
hand offs to treatment programs. Prescribing buprenorphine is one
of my favorite parts of my practice. Now that there’s no X waiver
required, we’re able to bring this safe and effective
treatment to our patients in a way that decreases their
mortality, all causes and opioid related by up to 50%. Getting Narcan into the right
folks hands. We know that one in seven kids
is going to be used in a reversal to save the life. Ultimately, I’m hoping that
emergency medicine can continue its trajectory towards a stigma
free environment for these patients. Patients with OUD and all of our
patients are worth saving. Thank you for being a lifesaver.
[Angadpreet “Preet” Sidhu] What needs to be
done more is to break down the stigma of medication to opiate, of
medications for opiate use disorders such as Suboxone. Narcan saves lives, but also
Suboxone saves lives as well.
Fentanyl Strips Save Lives
Dr. Edward Boyer provides a personal anecdote on how the use of fentanyl test strips saved many lives at a college campus party.
Transcript
[Edward W. Boyer] Hello everyone. My name is Ed Boyer
and I have a fentanyl story. So I’m an ER doc and a medical
toxicologist. So my area of sub specialization
is overdoses, poisonings, drug interactions and that sort of
thing. I also have a certain amount of
experience and background in the drug abuse world as well. Now, my daughter was going to
college at Syracuse University and I wanted to make sure that
she went off prepared. And one of the things that I did
was I got 5 fentanyl test strips from one of our harm reduction
colleagues at Ohio State. And I gave them to her. And my message was, I’m not
condoning. I’m not expecting you to use. I don’t expect you to
experiment. But if you ever wind up in a
situation where somebody gives you something and there’s a
temptation to use it, I want you to be safe by testing it with
these test strips. She goes off to college and time
passes, and she actually does well in college. So I’m pretty confident about
how things are going. And then in April of last year,
I got a text at like 2:00 in the morning from my daughter. And it said, essentially you
saved 300 people last night. One of the fraternities had
bought some pills and they gave them around to a whole bunch of
students. And when they got back to the
dorm, some of my daughter’s friends, “friends” wanted to use
them. So they used the fentanyl test
strips. They all contain fentanyl. You know, like, I I, I don’t
know exactly how accurate it is. I don’t know what reporting
happened, you know, the Panhellenic Council heard about
it afterward. But it highlights how the easy
availability of fentanyl test strips can save lives. And it also speaks to how a
broader based public health effort is necessary to help
minimize the the impact of, you know, like adulteration of all
sorts of substances with fentanyl.
Resources and Education
Bizzell US is proud to have created a variety of tools and resources for public use in conjunction with the National Institute of Drug Abuse Clinical Trials Network Dissemination Initiative, bringing researched based information to clinicians on a variety of topics related to substance use disorders. The links provided focus on the resources created specifically to address the opioid crisis.
Reducing the Risk of Fentanyl in the U.S. Video
We can work to decrease overdose deaths by increasing awareness of the dangers of illicitly manufactured fentanyl, learning how to discuss treatment options, and demonstrating how to respond to an overdose.
Reducing the Risk of Fentanyl in the U.S. Factsheets
Use these infographics, available in English and Spanish, to educate patients, families and communities about the dangers of illicitly manufactured fentanyl. Share the steps for recognizing and reversing overdose using naloxone.
English
https://nida.nih.gov/research-topics/trends-statistics/infographics/what-fentanyl
Spanish
https://nida.nih.gov/es/areas-de-investigacion/trends-statistics/infographics/que-es-el-fentanilo
Overdose Prevention Education for Clinicians Treating Patients with Opioid Use Disorder Video
This brief video offers strategies for overdose prevention through identification of an individual’s risk factors, stressing the importance of treatment adherence, safety planning, and overdose rescue preparation.
Overdose Prevention Education for Clinicians Treating Patients with Opioids for Chronic Pain
Treating patients with opioids for chronic pain includes the risk of development of opioid use disorder and overdose. This brief video offers strategies for avoiding onset of opioid use disorder as well as overdose prevention through identification of individual risk, safety planning and overdose rescue preparation.
The Case for Buprenorphine Initiation in the Emergency Department: Why, When, and How?
Listen and learn from nationally recognized experts in these 15-minute podcasts about the importance and effectiveness of starting buprenorphine treatment for opioid use disorder (OUD) in emergency departments.
https://www.mycme.com/pages/buprenorphine-initiation-in-the-emergency-department
Opioid Use Disorder in Emergency Departments
Learn best practices for patient-centered approaches to addressing opioid use disorder in the emergency department.
For more information about NIDA-CTN, please see:
https://nida.nih.gov/nidamed-medical-health-professionals/ctn-dissemination-initiative